编者按:6月28日,在第十届全国胃癌学术会议的“双语论坛2”专题研讨中,来自西安交通大学第一附属医院的樊林教授进行了题为“Crosstalk of Nerve and Cancer Cells in Perineural Invasion Contributes to Gastric Carcinoma Progression”的精彩演讲,《肿瘤瞭望》整理了其演讲内容,与读者分享。
在神经浸润中神经细胞和癌细胞的交联促进胃癌进展
Crosstalk of Nerve and Cancer Cells in Perineural Invasion Contributes to Gastric Carcinoma Progression
樊林 西安交通大学第一附属医院
胃癌(GC)是最常见的恶性疾病之一。近年来,胃癌患者术后生活质量和预后因微创治疗得以提高。迷走神经切除术时伤及迷走神经可导致腹泻和胆结石的形成。
D2胃远端切除的无保留神经的患者,其胆结石形成率可达30%以上,而对于平均人口约为10%,呈现出统计学意义。因此保留迷走神经的胃大部切除术减少了胃切除后综合征,即保留支配肝和胆道的前迷走神经干的肝分支以及后迷走神经干支配小肠的腹腔分支。研究表明,与LADG相比,保留迷走神经LADG,术后胆结石的发病率显著降低,并且两种术式的操作时间和出血几率相同。
那么问题是,保留神经是否适用于任何根治性远端胃切除的胃癌患者?
恶性肿瘤的一个关键特征是其从原发肿瘤转移至远隔部位。血管和淋巴是被广为接受的转移途径。还有什么不同的转移方式?肿瘤沿神经途径扩散在19世纪中期文献中已经描述,但研究相对较少。神经浸润(PNI)是肿瘤浸润神经的过程。它也被称为嗜神经癌扩散和神经蔓延。肿瘤细胞扩散至神经周围,是由肿瘤表达的分子与周围的基质细胞,以及与神经相关受体相互作用的过程。
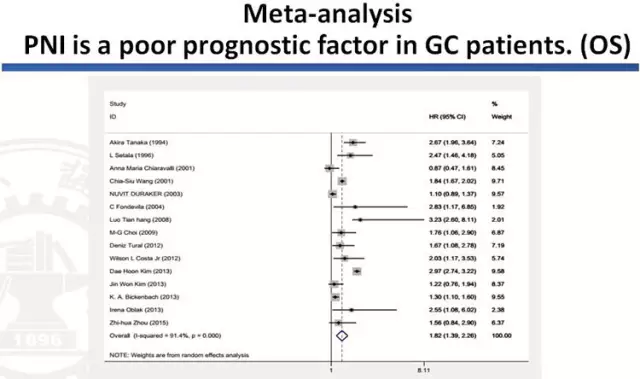
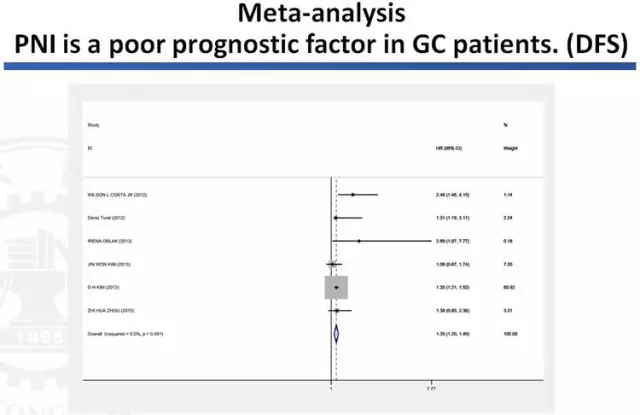
自2003年Duraker N在Surg Today上的报道,PNI已成为其他许多恶性肿瘤,包括胰腺、结直肠癌、前列腺癌和胆道癌的一个关键的病理特征。对于许多恶性肿瘤,PNI是预后不良的标志。因此,它在胃癌中具有同样的作用。荟萃分析发现PNI是胃癌患者包括OS和DFS预后不良的因素。一项荟萃分析纳入15项研究来自亚洲、欧洲、美洲等7706例胃癌患者,发现PNI是显著的预后不良的因素:OS(HR=1.82,95%CI:1.39-2.26,P <0.001);DFS(HR=1.35,95%CI=1.20-1.49,P <0.001)。
体外实验发现神经生长因子(NGF)在多种胃癌细胞系中高表达,胃癌细胞可刺激NGF的分泌。肿瘤细胞的侵袭呈嗜神经性。干扰神经生长因子,降低胃癌的侵袭能力。体内干扰NGF,使得坐骨神经功能和后肢足跨度(坐骨神经指数)幅度下降明显。在胃癌细胞系SGC7901的裸鼠成瘤实验中干扰NFG,肿瘤局限在接种灶,没有广泛的神经浸润,而对照组中,肿瘤表现出广泛的神经浸润。
保留迷走神经的胃切除在胃癌患者是一个有争议的问题。应该把握功能获益和根治性治疗的平衡。未来的发展需要更多的“大数据”和“精准医学”。
Gastric cancer (GC) is one of the most common malignancies. Recently, postoperative quality of life and prognosis of gastric cancer patients have been improved because of minimally invasive treatments. Injury to the vagal nerve during gastrectomy is known to cause postvagotomy diarrhea and gallstone formation.
The frequency of gallstone formation for D2 distal gastrectomy without nerve preservation can be above 30%, whereas that for the average population is about 10%,showing a statistically significant difference. Thus preserving vagal gastrectomy reduced gastric resection syndrome, during which, the hepatic branches of the anterior vagal trunk that innervate the liver and biliary tract, as well as the celiac branches of the posterior vagal trunk that innervate the small intestine are preserved. Studies have shown that, compared with LADG, reservations vagus nerve LADG, the incidence of gallstone significantly reduced, and both surgical operation time and the chance of bleeding are the same.
So the question is, is nerve preservation suitable for radical distal gastrectomy in any GC patients?
A key feature of malignant tumors is metastasis ability to distance. Vascular and lymphatic metastasis pathways are being widely accepted. Is there any different ways? Tumor spread that occurs in and along nerves has been described in the literature since the mid-1800s but has received relatively little research attention. Perineural invasion (PNI) is the process of tumor invasion nerves. It is also called perineural spread of cancer and neurological spread, during which tumors interact with surrounding stroma as well as receptors associated with peripheral nerves.
Since 2003, Duraker N reported in Surg Today’s, PNI has become a key pathological features in many other malignancies, including pancreatic, colorectal cancer, prostate and biliary cancer. PNI is a sign of poor prognosis for many malignancies. Therefore, it is same in gastric cancer. Meta-analysis found that PNI is a poor prognostic factor for OS and DFS in gastric cancer patients. A meta-analysis of 15 studies included 7706 cases of gastric cancer patients from Asia, Europe and America. PNI was found as a significant poor prognostic factor for OS (HR = 1.82,95% CI: 1.39-2.26, P <0.001) and DFS (HR = 1.35,95% CI = 1.20-1.49, P <0.001).
In vitro, nerve growth factor (NGF) is highly expressed in a variety of gastric cancer cell lines, Gastric cancer cells were able to stimulate neuron outgrowth. The migration of gastric cancer cells was linear, nerve-dependent, and polarized toward the ganglion. Interfere of NGF, reduced invasiveness of gastric cancer. Interference of NGF, so sciatic nerve function and hind foot span (sciatic index) rate declined significantly in vivo. In nude mice experiments of gastric cancer cell line SGC7901,Interference of NFG, confined tumor inoculation stove, without extensive perineural invasion, while the tumor showed a wide range of neural invasion in the control group.
Reserved vagus nerve gastrectomy in gastric cancer patients is a controversial issue. The benefits and curative treatment function should be balanced. Future development needs more "big data" and "precision medicine."





 京公网安备 11010502033352号
京公网安备 11010502033352号